The Quality Expo is an opportunity for improvement projects created by employees to be shared as part of the Henry Ford Health culture of continuous process improvement.
For more information, visit https://onehenry.hfhs.org/departments/qualityandsafety/Pages/Quality-Expo.aspx
-

Project #32: Improving Patient Reported Outcome Survey Completion Rate in Elective Hip and Knee Replacements
Tammy Krozal, Jennifer Pietsch, Michael Motherwell, Eric Makhni, William Dobson, Lisa M. Schley, Barb Babb, Michael Charters, Thomas L. Schoen, and Tori Davis
Problem Background: Patient Reported Outcomes Surveys (PROS) are not being completed at a high enough rate. PROS provide a direct report of the patient experience and facilitate patient outcome projection, identify areas for quality improvement and can offer early detection of implant failure. Our goal was to improve the rate of both pre and post operative survey collection while also making survey results available to a broader audience.
... Read More -

Project #33: Achieving Commission on Cancer Operative Standard 5.8 for Primary Lung Cancer Resections
Brian J. Green, Ikenna C. Okereke, Miguel Alvelo-Rivera, Corbin Cleary, and Andrew M. Popoff
Introduction: Compliance with the Commission on Cancer (CoC) Operative Standard 5.8 Pulmonary Resection results in longer patient survival and better surgical outcomes. The CoC operative standard calls for all curative intent lung cancer resections to have at least 3 mediastinal lymph node stations in addition to at least 1 hilar station sampled at the time of resection at a minimum rate of 80%. Our project aim was to meet... Read More
-

Project #34: Initial Clostridioides difficile Testing
Tatiana Assenova, Cathleen McCloskey, Sarah Prascius, and Alex K. Wells
Problem Statement: First Floor GPU (General Practice Unit) at Henry Ford West Bloomfield Hospital experienced an increased number of hospital acquired Clostridioides difficile infections in Q1 and Q2 of 2023. Many of those cases occurred because there was a delay in testing due to length of time between stooling and testing within the first three days of hospital admission, which is the community onset window. Improvement Statement: Design new... Read More
-

Project #35: Using a Digital Mental Health Tool to Curb Access Issues to Mental Health Services
Shamole Ahmed, Franciosa Gavino-Collins, Jordan M. Braciszewski, Doree A. Espiritu, Cathrine Frank, Amanda May, and Tiffeny Jones
BHS aims to offer 100% of patients referred to Adult Behavioral Health Integration (BHI) a digital mental health tool (Thrive) that provides therapeutic support to initiate treatment while waiting for an appointment and hopes to improve mental health outcomes and quality by 5% and enroll at least 10% of patients offered the tool into the program by Nov. 1, 2023. Plan/Current State: Henry Ford Behavioral Health receives 700 referrals... Read More
-

Project #36: Increasing 2 out of 3 Smoking Cessation Interventions for Vascular Surgery Patients
Paul Corcoran, Millanie Villareal, and Amanda Holm
Aim: By December 31, 2024, ≥25% of tobacco smoker patients of HFH Detroit vascular surgery will receive 2 out of 3 smoking cessation interventions: 1) Physician delivered advice 2) Nicotine Replacement Therapy 3) Referral to smoking counseling services. Plan/Current State: In 2022 the most common smoking cessation practice was through physician delivering advice to stop smoking. However, physician advice alone will not count towards the Smoking Cessation Vascular Surgery... Read More
-

Project #37: Outpatient Rehabilitation Fall Prevention: Working Towards a Safer Journey
Laura Agemak, Nicole Robinson, Jill Norander, Vaishnavi Srivatsan, and Shailly Prabhakar
Aim: Patient falls within the Rehab Services outpatient clinics are the primary safety event reported through the Henry Ford Health R/L process. According to the report from the American Physical Therapy Association from September 2023, "The Economic Value of Physical Therapy in the United States" the average cost savings for fall prevention programs is estimated to be $2144 per Episode of Care. For these reasons, fall reduction was set... Read More
-

Project #38: ClinicalTrials.gov: building compliance within HFH
Kayliegh McEachren, Stephanie Marl, Tiffany Pearce, and Sonia Carrillo
Clinicaltrials.gov became publicly available in 2005 and was created as a resource for patients, physicians, regulatory bodies, and funders to provide the most up-to-date information about clinical trials conducted throughout the nation. Although motivated to comply with regulations, those tasked with maintaining records, found the website to be cumbersome and this has resulted in thousands of poorly maintained records. The Food and Drug Administration (FDA), has begun informing institutions... Read More
-
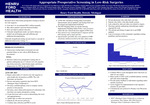
Project #39: Appropriate Preoperative Screening in Low-Risk Surgeries
Pat Patton, Rupen Shah, Marianne Franco, Cletus Stanton, Lynda Lopis, Kelsey Sale, Sicknee Daher, Jacqueline J. Machnacki, Kelly Bourn, and Jessica Wren
Background: Research shows that routine preoperative testing in elective low risk surgeries: Costs the U.S. an estimated $85.2 million annually; May add to patient’s personal financial burden; Does not improve patient outcomes; Clinically insignificant results can lead to delays in needed care prolonging pain and suffering and additional decompensation.
Clinically insignificant testing can also lead to a cascade of additional unnecessary testing.
PROBLEM STATEMENT: Unnecessary testing leads to increased... Read More
-

Project #41: Creating a Safe Space to Care and Heal in an Inpatient Psychiatric Hospital, Utilizing Welle and Empowering De-Escalation, a Hands Off Approach to Care
Emily Sexton, Tasmiyah N. Gaskins, Elizabeth Travis, Vahid Pasovic, Mary Rogers, Therese Samarco, Athena Hinojosa, and Jackie Harrington
Incidence of violence often occur in the psychiatric setting during physical management events which include: Physical hold, restraint or seclusion. At Kingswood Hospital the switch from CPI de-escalation and physical management to Welle De-escalation and physical management experienced interruptions and had observed opportunities for expansion, buy-in and development towards improved clinical care. In late 2021 incidence of patient reported abuse after physical holds led to investigation noting team members... Read More
-

Project #42: Improving Documentation for Trauma Patients in the Emergency Department
Michelle Ring, Lisa Simpson, and Vanessa L. Wargosie
Problem Statement: Staff turnover and lack of standardized processes led to missing documentation and inefficient management of trauma patients. The RNs in the ED at HFWH need education, support, consistency, and prompt feedback to ensure high quality trauma care that meets American College of Surgeons (ACS) national benchmarking standards. In previous years, overall trauma documentation for vital signs and GCS were below the national trauma standard of 90% and... Read More
-

Project #43: Combating Workplace Violence: The Implementation of a Behavioral Emergency Response Team
Jessica Schmidt
Workplace violence, patient, and staff safety continue to be a top priority and concern for Henry Ford Jackson Health (HFJH). Evaluating the current process at HFJH, there was no formal process to support clinical staff members to maintain patient and staff safety during acute behavioral health crises on medical inpatient units prior to the activation of a “Security Assistance”, or security personnel response to situations involving an actual or... Read More
-

Project #44: OPIOID HARM REDUCTION: Increasing Naloxone Distribution at ED Discharge
Heather Faraone, Thomas Fagan, John Joseph, Joe Miller, Nancy MacDonald, and Jacob Manteuffel
Background: Deaths from opiate overdose remain a persistent public health crisis. Of the 11,557 patients discharged from the Emergency Department (ED) with non-fatal opioid overdose, one year mortality shows 5.5% died within one year; 20.5% died within the first month; 22.4% died within the first two days. Naloxone can rapidly reverse fatal overdose and reduce mortality when available in the community. Identify people at risk for overdose, intervene to... Read More
-

Project #45: Unit-based Training Program for Ultrasound-Guided Peripheral Intravenous Catheter Insertion
Kristina Boudreau and Sarah Bledin
Introduction: Peripheral intravenous catheters (PIVs) are routinely utilized for infusions of medications and/or fluids in the healthcare setting. PIVs vary in length, gauge (catheter diameter), and other properties such as radiopaque guidewires, flexible guidewires, etc. The placement site, catheter length, and diameter is selected by the healthcare personnel inserting the PIV. The healthcare personnel inserting PIVs varies across institutions, but registered nurses insert most PIVs in the hospital setting.... Read More
-

Project #46: Enhancing the Sepsis Narrator Tool to Improve Patient Care and Outcomes
Suzanne Schlacht, Heatha Bailey, Darinda L. Blaskie, Ronnel G. Miranda, Tanya Larocque, Cynthia Valerio, Jean Kokochak, and Namita Jayaprakash
Background: The SEP 1 bundle is evidence based best practice guidelines for the management of patients with severe sepsis and septic shock. Compliance with SEP 1 bundled care is monitored by CMS and publicly reported. When all required SEP 1 bundle elements are delivered within timing specifications of 3- and 6-hours, patient outcomes demonstrate lower mortality, fewer complications, and a reduction in length of stay.
Problem statement: At Henry... Read More
-

Project #47: Centralization of Clinical Trial Budgeting has Resulted in Optimization
Jennifer Fowler, Karie Gignac, and Tiffany Pearce
Introduction: Fee schedules used to negotiate clinical trials budgets across the health system have historically been very different. Clinical care fees are standardized based on the hospital charge master, however administrative fees for staff time and effort have been extremely variable due to a decentralization approach. This has resulted in sub-optimal budget negotiations for clinical trials due to multiple factors: Under-estimation of costs; Lack of trained staff in each... Read More
-

Project #48 Advancing Pharmacy Advantage Processes through Automation
Scott Backman, Zade Shammout, Sweta Patel, Amanda T. Soyad, and Dawn Hall
Aim: It is essential to develop automation at Pharmacy Advantage Specialty Pharmacy on an ongoing basis to enhance business operations. This project aims to assess the impact of several automated solutions put in place at Pharmacy Advantage to help advance our practice. The focus of this project is to reduce costs, errors, and employee time on manual processes. The goals differ among all solutions developed but aim for a... Read More
-

Project #49 Transplant Psychology Post-Liver Transplant Follow-up Clinic
Antú Segal
Abstract: Liver transplant is a life-saving option for patients with end stage liver disease. The journey to transplant and post-liver transplant is complicated and can be a challenge to patients and their families. The prevalence and connection between medical, psychological, and social factors that impact post-liver transplant patients warrants further investigation. Routine follow-up of post-liver transplant patients has helped in identifying and mitigating risks that impact surgical outcomes. AIM:... Read More
-

Project #50: Utilization of PIC Score to reduce ICU utilization in patients with chest injury
Shanen Beck, Sara Glowzinski, Marianne Franco, and Maria Schneider
Aim: To achieve 10% reduction in ICU utilization for chest injured patients at West Bloomfield Hospital, while maintaining 0% adverse event rate attributable to placement in a lower acuity setting within 12 months of implementation.
-

Project #51: Reducing Hypertension in Younger African American Men: Advancing Health Equity with a Multidisciplinary Express Blood Pressure Clinic
Mike Anderson, Michelle Buggs, Roberta Eis, DaWanna Jones, Sarah Kolander, Sanjeev Kumar, Carolyn Lang-Piontkowski, Melissa Little, Alison Lobkovich, Pamela Shabazz, Octavia Solomon, and Denise White-Perkins
Background/Aim: The African American (AA) population is disproportionately impacted by hypertension-related complications. Compared to other races, AAs are at a significantly higher risk of mortality and a three-times increased risk of stroke. AA men have the highest hypertension-related mortality compared to any other race, ethnic group, or sex. In response to this challenge, the American College of Preventive Medicine (ACPM) collaborated with the Centers for Disease Control (CDC) to... Read More
-

Project #52: Process Improvement in Interventional Research Through Utilization of a Clinical Trials Management System (CTMS)
Kenneth Winters, Hannah Eaton, Travis Wheeler, and Amanda Wigand
Introduction: Until recently, the management of clinical trials at Henry Ford Health has been largely decentralized, creating a disparity in trial administration and oversight from study to study. Individual departments and study teams were responsible for determining how their interventional research would be organized and conducted. This led to a vast variation in the way that Henry Ford researchers tracked and maintained research portfolios, study records, subject participation, as... Read More
-

Project #53: Clinical Decision Unit (CDU)
Anna Leszczynski, Elizabeth F. Ashley, Kristina M. Cross, Wendy Butterfield, Ghazwan Atto, Ghassan Atto, Toni Silas, Elizabeth Plemmons, and Ryan Spencer
Aim: Focused action plan to decrease observation patients’ length of stay (LOS) supporting increased hospital bed capacity. The goal is for decision to discharge as observation or admission occurring under 23 hours of placement. This reduction in LOS will result in expanded site capacity, decreasing holding hours for all admitted and observation patients bed placement. Observation LOS at other observation units at Wyandotte Hospital from October 2022-November 2023 average... Read More
-

Project #54: An Individualized Unit Based Approach to Utilizing Pressure Injury Prevention Strategies for Acute Care Nursing Staff
Cindy Schleis, Hailey Berlin, Mackenzie Morencie, Nancy Price, Swati Verma, Dana Y. Johnson-Meah, and Cherie Sweet
Hospital Acquired Pressure Injuries (HAPI) are a complex and important safety issue. They increase length of stay, readmission rates, costs , and mortality. Per NPIAP Pressure Injury (PI) Fact Sheet- 2019: Avg cost per patient for HAPIs: $29,000-$151,700; 2.5 million patients develop PI and 60,000 die annually. At HFH Detroit, HAPI rates from Jan to Aug 2022 peaked to 6.5% (NDNQI* mean 2021 Q1 benchmark is 2.9%). Increased HAPI... Read More
-
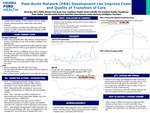
Project #55: Post-Acute Network (PAN) Development can Improve Costs and Quality of Transition of Care
Gloria Rey, Susan Craft, Audra Stoker, and Anna Bloemen
Aim: Change referral patterns to focus patient choice on quality; Improve partnering facility relationships with system hospitals; Promote utilization of facilities that collaborate with health system on quality improvement projects, meetings, quality reports, patient care. Problem Statement: Historically patients/families have selected facilities based on location, continuation of care with providers, feedback from friends/family; CMS 2019 Final Ruling required that quality data/information be provided with the intent to guide patients... Read More
-

Project #56: HFH Acute Care PT and OT Throughput Initiative
Adele Myszenski, Paula Kane, Romina Bello, Tiji Avirah, Jennifer Trimpe, Justine Kenyon-Nitch, Don Frega, and Sal Lograsso
Problem #1: Rehab lacks qualitative metrics for Key Performance Outcomes. Problem #2: Improving Rehab throughput/appropriate utilization would assist in decreasing LOS for the patient.
Aims: Improve TAT and Frequency to in turn improve Rate of DC to post-acute facility in turn to reduce LOS; reduce demand for services deemed unnecessary / see more of “right” patients; reduce demand for follow ups per therapist prescription (educate and train at time... Read More
-

Project #57: Transforming Atrial Fibrillation Care in the ED: A Quality Improvement Initiative for Safe and Streamlined ED Transitions of Care
Arfaat Khan, Satheesh Gunaga, Christian P. Fisher, Sue Piatak, Ryan T. Shelters, Timothy Stevens, Kaitlyn Hanlon, Jacob Babel, Alyssa Wood, Layan El-khatib, Brunda L. Kumar, Mohammad H. A Ayoub, Dennis Smythe, Bethany Dalessandro, Ryan Spencer, and Elizabeth Plemmons
ED Atrial Fibrillation (A-FIB) Treatment Protocol Implementation: Implement a focused ED A-FIB treatment protocol to achieve effective rate control using a combination of IV and oral medications. This aims to optimize the management of A-FIB presentations in the emergency department. Improvement in Outpatient Transitions of Care: Enhance the safety around outpatient transitions of care for A-FIB patients. This includes designing protocols for the safe discharge of patients with expedited... Read More


